Patient Activation: The Best Kind of Self Help

What is patient activation anyway?
Terms like “patient engagement,” “digital health” and “customer experience” are thrown around a lot, and even though they’re used interchangeably, they have different meanings— ranging from wearing a fitness tracker, logging onto an online portal or getting appointment reminders via text. All of these concepts are related to a healthcare organization trying to improve patient satisfaction and patient outcomes.
Patient activation; however, is focused on putting this power in the hands of the patient. Patients can be engaged in conversations during doctor visits, dutifully reading brochures, or even searching for things on the internet—but being activated means doing more than those one, two or three things.

Patient activation is understanding one’s role in the care process and having the knowledge, skills, and confidence to manage one’s health and health care.1 It is comprised of the actions individuals must take to obtain the greatest benefit from the health care services available to them to maximize his or her own health.2
For activated patients, this behavior becomes a way of life. For example, after a doctor appointment, an activated patient will go home and try to understand what the doctor said, do whatever they can to educate themselves further, and keep track of their symptoms. This type of diligence is beneficial and can help improve their quality of life, especially for those with chronic conditions.
Why does patient activation matter?
One in four Americans have multiple chronic conditions, those that last a year or more and require ongoing medical attention or that limit activities of daily living.4
People with chronic conditions are the most frequent users of healthcare in the U.S. They account for 81% of hospital admissions; 91% of all prescriptions filled; and 76% of all physician visits.5
133 million Americans – 45% of the population –
have at least one chronic disease.3
Chronic conditions are tough. They’re tough to diagnose, tough to manage, tough to maintain a positive attitude about, and certainly tough to experience. Because managing these conditions can be intimidating and overwhelming, patients often take a back seat and wait for their physician to figure it out for them. Our healthcare teams can only do so much; they’re never going to be a better advocate than the patients themselves. There is an opportunity to change the overall healthcare experience and improve outcomes by activating patients sooner in the care pathway – educating them and giving them access to tools to make informed steps for managing their condition.
“Highly activated patients are two or more times as likely as those with low activation levels to prepare questions for a visit to the doctor; to know about treatment guidelines for their condition; and to seek out health information, including comparisons of the quality of health care providers. ”6
From passive to active
So how do you activate more patients? And how do you ensure it will be effective? We think it starts with bringing the patient into the conversation — and learning from those experiences.
You must define your audiences, identify the gaps in their respective journeys and deliver the right message to the right individual through the appropriate channel. Understanding the uniqueness of each individual, pinpointing critical moments and tailoring content accordingly is critical when advancing patients inside the care pathway.
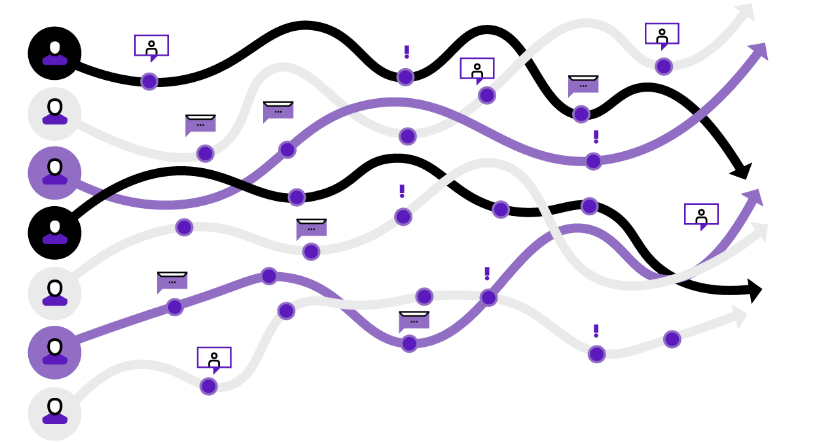
We create and implement customized marketing communications to reach patients and boost their understanding of and confidence in therapy choices. This results in positive health behaviors and ultimately, better outcomes. And it doesn ’t end there—while we ’ re focusing on individual interactions, it’ s important to learn from them and scale those enhancements to larger groups.
Once patients are successfully activated, it’s just as important to keep them activated. We must constantly be evolving. Patient activation requires a behavior change within a complex ecosystem of care—and while consumers wait for payors, providers, and data systems to become more integrated, we are here to help consumers connect the dots for themselves.
1Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers.Health Serv Res. 2004 ; 39 ( 4 Pt 1 ): 1005 – 26.
2http://www.cfah.org/pdfs/CFAH_Engagement_Behavior_Framework_current.pdf
3Wu S, Green A. Projection of Chronic Illness Prevalence and Cost Inflation. RAND Corporation, October 2000.
4Multiple Chronic Conditions—A Strategic Framework: Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions. Cdc-pdf External Washington, DC: US Dept. of Health and Human Services; 2010. Accessed November 18, 2014.
5Partnership for Solutions. Chronic Conditions: Making the Case for Ongoing Care. September 2004 Update. Available at: http://www.rwjf.org/files/research/
6Fowles JB, Terry P, Xi M, Hibbard J, Bloom CT, Harvey L. Measuring self-management of patients’ and employees’ health: further validation of the Patient Activation Measure (PAM) based on its relation to employee characteristics. Patient Educ Couns. 2009 ; 77 ( 1 ): 116 – 22.